It’s not uncommon to feel a burning sensation in your chest or discomfort in your upper abdomen after a heavy meal, but identifying the root cause of that discomfort is important for finding relief and preventing complications. Two common conditions—gastric pain and acid reflux—are often confused because their symptoms can overlap.
However, they have different triggers, underlying mechanisms, and treatment approaches. This article will help you understand the key differences so you can better manage your symptoms and seek the right medical care when needed.
Understanding Gastric Pain
Gastric discomfort typically refers to discomfort in the upper abdomen, especially in the area just below the breastbone. It’s commonly caused by issues affecting the stomach lining, such as gastritis, peptic ulcers, or even stomach infections like Helicobacter pylori. This type of pain is often described as a dull, burning, or gnawing sensation. It may get worse on an empty stomach and improve after eating, although this can vary depending on the underlying cause.
People who experience gastric cramps might also report bloating, early satiety (feeling full quickly), nausea, or a sense of heaviness after meals. Triggers often include stress, excessive use of painkillers like NSAIDs, alcohol, spicy foods, or bacterial infections.
When gastric pain is persistent or worsens over time, it’s important to see a doctor. Chronic inflammation of the stomach lining or ulcers can lead to complications such as bleeding, anemia, or, in rare cases, an increased risk of stomach cancer.
What Is Acid Reflux?
Acid reflux, also known as gastroesophageal reflux disease (GERD) when it becomes chronic, is a condition where stomach acid flows backward into the esophagus. This happens when the lower esophageal sphincter (a muscle that separates the stomach from the esophagus) becomes weak or relaxes inappropriately.
The hallmark symptom of acid reflux is heartburn—a burning sensation behind the breastbone that can rise into the throat. Other common signs include a sour or bitter taste in the mouth, regurgitation of food or acid, chest pain that can mimic heart-related pain, and difficulty swallowing. Unlike gastric pain, acid reflux is more likely to be triggered or worsened by lying down after eating, wearing tight clothing, or consuming acidic foods like coffee, tomatoes, and citrus.
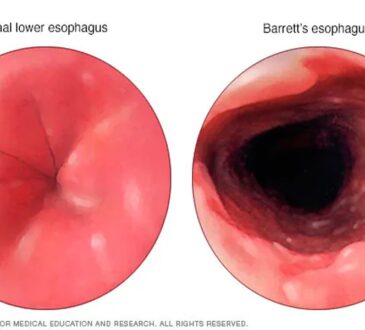
Long-term acid reflux can damage the lining of the esophagus and increase the risk of conditions such as esophagitis, strictures, or even Barrett’s esophagus, a precancerous change in the esophageal lining.
How to Tell Them Apart
While both gastric pain and acid reflux may cause upper abdominal discomfort, the location, triggers, and accompanying symptoms can help distinguish them. Gastric pain is usually localized to the stomach area and may be tied to meal timing, especially when the stomach is empty.
Acid reflux, on the other hand, is more commonly felt as a burning sensation that travels upward toward the chest or throat and is often worse after meals or when lying flat. Another distinguishing factor is the presence of regurgitation and sour taste, which are classic signs of acid reflux but not typically associated with gastric pain.
If your symptoms include these features, GERD is more likely. That said, it’s also possible for both conditions to coexist. For instance, someone with gastritis may also have acid reflux, making it harder to isolate the cause of symptoms without medical evaluation.
When to Seek Medical Help
Occasional heartburn or mild gastric discomfort might not be cause for concern, especially if it responds well to over-the-counter remedies like antacids. However, you should see a healthcare provider if your symptoms occur frequently, persist for more than a few weeks, or are accompanied by alarming signs such as unintended weight loss, persistent vomiting, black or bloody stools, or difficulty swallowing. In such cases, diagnostic procedures like gastroscopy (endoscopy) may be recommended to examine the stomach and esophagus and identify the root cause of your symptoms.
Treatment and Lifestyle Adjustments
Both gastric pain and acid reflux are manageable with the right approach. For gastric pain, treatment may involve proton pump inhibitors (PPIs) or H2 blockers to reduce stomach acid, antibiotics if an infection like H. pylori is present, and dietary changes to avoid irritation. Eating smaller, more frequent meals and avoiding alcohol or painkillers can also help protect the stomach lining.
For acid reflux, lifestyle changes play a significant role in symptom relief. Elevating the head of your bed, avoiding large meals before bedtime, quitting smoking, and losing excess weight can make a big difference. Medications like PPIs or antacids are often effective, but long-term use should be monitored by a doctor.
Conclusion
Although gastric pain and acid reflux can feel similar, they stem from different causes and may require different treatments. Recognizing the differences in symptoms, triggers, and patterns of discomfort can help you and your doctor pinpoint the issue more accurately. If you’re frequently troubled by either gastric pain or signs of acid reflux, don’t ignore it—early management is key to preventing more serious complications and improving your quality of life.