Spinal fracture surgery depends not only on surgical skill, but also on the quality of the implants used to stabilize the spine. Screws, rods, cages and plates form the mechanical foundation of many procedures, and advances in materials science are reshaping their effectiveness. Dr. Larry Davidson, an advocate for minimally invasive procedures, has noted that modern implants are being engineered with coatings, composites and resorbable designs that improve fusion rates, reduce complications and align better with the body’s natural healing processes.
The rise of next-generation implants reflects a shift from hardware that merely holds the spine together, to devices that actively participate in healing. With innovations in metals, polymers and biologically active coatings, materials science is expanding the possibilities for safer and more durable fracture repair.
Titanium and Its Advantages
Titanium has long been a preferred material for spinal implants. Its strength-to-weight ratio, resistance to corrosion and bio-compatibility make it ideal for rods, screws and cages. Unlike stainless steel, titanium is less likely to interfere with imaging, allowing for clearer post-operative CT or MRI scans.
Newer titanium alloys are designed to be even more durable, while maintaining flexibility. It reduces stress on the bone-implant interface, decreasing the risk of loosening or failure. For many patients, titanium remains the foundation of spinal stabilization.
PEEK and Polymer Implants
Polyetheretherketone (PEEK) is a polymer increasingly used in interbody cages. Its stiffness is closer to that of natural bone, which reduces stress shielding, a problem where bone weakens because the implant carries too much of the load. PEEK also allows for radiographic visibility, making it easier for surgeons to monitor fusion.
Some PEEK implants are enhanced with coatings or fillers to improve bone integration, addressing one of the material’s main limitations. By balancing strength, flexibility and imaging compatibility, PEEK continues to gain ground in spinal surgery.
Biologically Active Coatings
One of the most exciting advancements in implant technology is the use of biologically active coatings. Hydroxyapatite, a mineral naturally found in bone, can be applied to implants to encourage bone growth at the surface. Porous titanium coatings create textured surfaces that allow bone to grow directly into the implant, enhancing stability.
Antibacterial coatings are also being developed to reduce the risk of infection, a significant concern in complex fracture repairs. These coatings release agents that prevent bacterial adhesion, while maintaining compatibility with bone cells. Coatings turn implants into active participants in healing, rather than passive devices. This approach supports faster fusion and reduces complications.
Resorbable Implants
Resorbable implants represent a major step forward in spinal surgery. Made from polymers or composites designed to degrade over time, these devices provide temporary stabilization, while the bone heals. Once fusion is achieved, the implant dissolves, leaving behind only the patient’s natural anatomy.
These implants help lower the risk of long-term complications linked to permanent hardware, including irritation, loosening or the need for revision surgery. They show particular promise for younger patients, where maintaining long-term spinal health is essential. Research continues to confirm that resorbable implants remain strong enough to support healing, before safely breaking down.
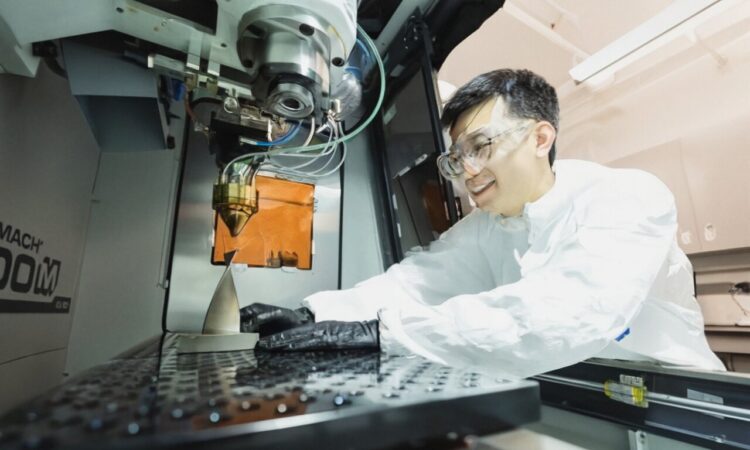
3D-Printed Custom Implants
Advances in 3D printing allow for patient-specific implants designed directly from CT or MRI scans. These custom devices match the patient’s anatomy precisely, improving fit, stability and load distribution.
3D-printed implants can incorporate porous structures that mimic natural bone, encouraging integration. Surgeons can also design implants tailored to complex fracture patterns, that standard hardware cannot address. For patients with unusual anatomy or extensive damage, custom implants offer solutions that once seemed impossible.
Balancing Strength and Flexibility
The challenge in implant design is balancing strength with flexibility. Implants must stabilize the spine, without overburdening bone, which can lead to stress shielding or non-union. New materials and hybrid designs aim to strike this balance, providing support that works in harmony with the body’s natural biomechanics. By combining metals, polymers and biologic coatings, next-generation implants create systems that adapt to patient needs. This adaptability is particularly important in fracture surgery, where bone quality and healing potential vary widely.
Dr. Larry Davidson remarks, “There’s still work to be done, but we’re on the right path.” His words reflect the reality of implant innovation. While advances in coatings, resorbables and 3D printing show enormous promise, ongoing research and refinement remain essential to fully realize their potential in everyday surgical practice.
Athletes and Next-Gen Implants
Athletes recovering from spinal fractures often place higher demands on implants. The need for stability during intense activity requires materials that are strong, yet flexible enough to support performance. Titanium alloys and coated implants provide the durability athletes need, while biologically active designs enhance fusion rates.
Resorbable implants may also prove valuable for younger athletes, allowing stabilization during healing, without long-term interference. Athletes benefit greatly from these innovations, which align surgical repair with the demands of performance and mobility.
Training Surgeons in Implant Innovation
As implants become more advanced, surgical training must develop. Surgeons must learn not only how to place hardware, but also how to select the best materials for each patient. Mentorship and simulation training expose younger surgeons to the nuances of implant choice, from titanium and PEEK to biologically active and resorbable devices.
Reducing Risks with Next-Gen Designs
Next-generation implants are also designed to reduce risks. By improving integration with the bone, they decrease the chance of loosening. By incorporating antibacterial coatings, they reduce infection risks. Resorbable options eliminate complications associated with permanent hardware. These innovations reflect a shift toward proactive complication prevention. Patients benefit not only from stronger repairs but from safer long-term outcomes. The future of materials science in spinal surgery is rapidly advancing.
Smart implants capable of transmitting data about load, alignment or fusion progress are already being tested. These devices may one day allow surgeons to monitor healing remotely, adjusting rehabilitation plans based on real-time feedback. As biologically active materials, resorbable polymers and custom 3D printing mature, implants will become more personalized and more effective. The line between hardware and healing will continue to blur, with implants serving as both stabilizers and biological partners in recovery.
Materials science is reshaping spinal fracture surgery through titanium alloys, PEEK polymers, biologically active coatings, resorbable devices and custom 3D printing. These innovations strengthen repairs, promote healing and reduce complications. The experience highlights the importance of using implants not only as tools of stabilization, but as allies in biological healing. This work reflects a future where materials science and surgical skill work hand in hand, providing patients with safer, more effective, and more personalized care.