Barrett’s esophagus is a condition that affects the lining of the esophagus – the tube that connects the mouth to the stomach. It occurs when chronic acid reflux, or gastroesophageal reflux disease (GERD), damages the normal tissue, causing it to change into tissue similar to that found in the intestine.
While Barrett’s esophagus itself does not always cause noticeable symptoms, it can increase the risk of developing esophageal cancer. Early detection is crucial, and one of the best diagnostic tools available for identifying this condition is a gastroscopy procedure.
Understanding Barrett’s Esophagus
Barrett’s esophagus develops when stomach acid repeatedly flows back into the esophagus, irritating and damaging its lining. Over time, the body replaces the normal squamous cells with columnar cells, which are more resistant to acid but also more prone to abnormal changes.
The main risk factor for Barrett’s esophagus is chronic acid reflux. People who experience frequent heartburn, regurgitation, or a sour taste in the mouth are more likely to develop it. Other risk factors include smoking, obesity, older age, and a family history of esophageal disease.
While the condition often does not cause symptoms distinct from GERD, its potential to progress to esophageal adenocarcinoma makes regular screening and monitoring essential.
The Role of Gastroscopy in Diagnosis
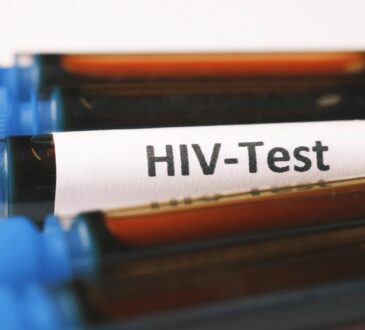
A gastroscopy test is a minimally invasive procedure that allows doctors to look directly inside the esophagus, stomach, and the upper part of the small intestine. It involves inserting a thin, flexible tube with a camera – called an endoscope – through the mouth and down the throat.
During the procedure, doctors can visually inspect the esophagus for signs of damage, inflammation, or abnormal tissue. If suspicious areas are detected, small tissue samples (biopsies) can be taken for microscopic examination. This biopsy is what confirms the diagnosis of Barrett’s esophagus and determines whether any precancerous changes, known as dysplasia, are present.
Gastroscopy is usually performed under light sedation, ensuring that patients remain comfortable and pain-free throughout the procedure. The entire process typically takes less than 15 minutes, and most patients can return home the same day.
What Doctors Look for During the Procedure
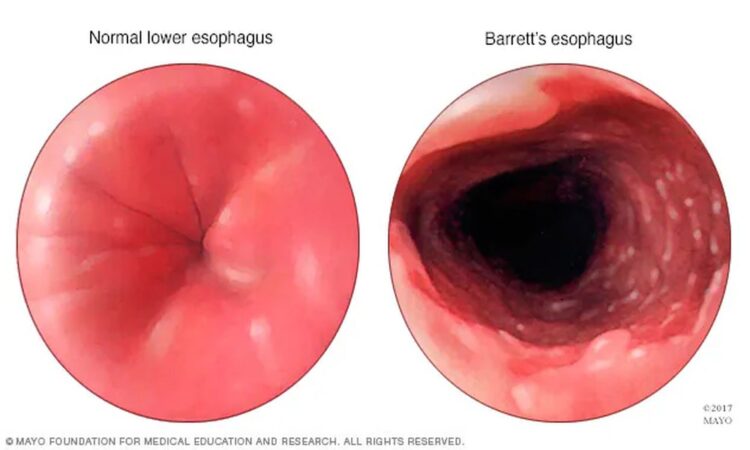
When examining the esophagus, doctors look for characteristic color and texture changes in the lining. Normal esophageal tissue appears pale and smooth, while Barrett’s tissue often looks reddish and velvety, similar to the lining of the intestine.
If these visual changes are seen, multiple biopsies are taken to confirm the diagnosis. Pathologists then analyze the tissue samples under a microscope to detect intestinal-type cells or precancerous abnormalities.
The results help classify the condition into different stages – ranging from non-dysplastic Barrett’s (no abnormal cells) to low-grade or high-grade dysplasia. Identifying the stage is critical, as it determines how closely the patient should be monitored and whether further treatment is needed.
When to Get Tested
People with long-term acid reflux, especially those who have had symptoms for more than five years, are advised to talk to their doctor about screening. Men over the age of 50 who are overweight, smoke, or have frequent GERD symptoms are particularly at risk.
In many cases, Barrett’s esophagus is discovered during a gastroscopy performed for other reasons, such as investigating persistent heartburn, difficulty swallowing, or unexplained nausea. If you belong to a high-risk group, regular check-ups and follow-up endoscopies can help detect changes early before they progress to cancer.
Managing Barrett’s Esophagus After Detection
Once Barrett’s esophagus is diagnosed, the next step is to manage the underlying acid reflux and monitor the condition over time. Lifestyle modifications, such as maintaining a healthy weight, avoiding large meals, reducing caffeine and alcohol intake, and quitting smoking, can significantly reduce symptoms and prevent further damage.
Medications that reduce acid production, like proton pump inhibitors (PPIs), are commonly prescribed to control GERD symptoms and minimize irritation to the esophagus.
For patients with dysplasia or early cancerous changes, treatments may include endoscopic procedures such as radiofrequency ablation or endoscopic mucosal resection, which remove or destroy abnormal cells without the need for major surgery.
Regular monitoring through repeat gastroscopy ensures that any new or worsening changes are caught early, improving long-term outcomes.
The Importance of Early Detection
Early detection of Barrett’s esophagus can be life-saving. Because the condition itself often causes few or no symptoms, many people remain unaware they have it until it has progressed to more serious stages. Routine medical checkups and open communication with your healthcare provider are key to preventing complications.
Detecting Barrett’s esophagus early allows for effective treatment and significantly reduces the risk of developing esophageal cancer. Patients diagnosed in the early stages have an excellent prognosis when managed properly with medical therapy and surveillance.
Conclusion
Barrett’s esophagus is a silent but serious condition that develops as a result of long-term acid reflux. Left unchecked, it can increase the risk of esophageal cancer, making early detection and management essential.
Through gastroscopy, doctors can accurately diagnose Barrett’s esophagus, assess the severity of tissue changes, and develop a tailored treatment and monitoring plan.
If you experience chronic heartburn or have risk factors for GERD, it’s important not to ignore your symptoms. Consulting a gastroenterologist and undergoing appropriate screening can provide peace of mind – and potentially save your life through early intervention.